A new molecule, without disproportionate risks for the health of patients, allows treatment of the rapidly progressing form of sleeping sickness
Transmitted by the notorious tsetse fly, sleeping sickness is still potentially deadly if not treated in time. But on top of that, the drug used until now to combat the acute stage of this parasitic infection caused the death of 5 to 10% of patients due to violent adverse effects. A newly discovered molecule has changed everything: research has demonstrated that it is effective and safe in all forms and all stages of the disease.
“Clinical trials to which we contributed recently established that fexinidazole treats the neurological stage of rhodesiense human African trypanosomiasis, but without causing serious adverse events as was too often the case with melarsoprol I. These trials guided the new treatment recommendations recently published by the World Health Organization,” states Veerle Lejon, IRD biochemist at the INTERTRYP laboratory.
Two stages, two forms
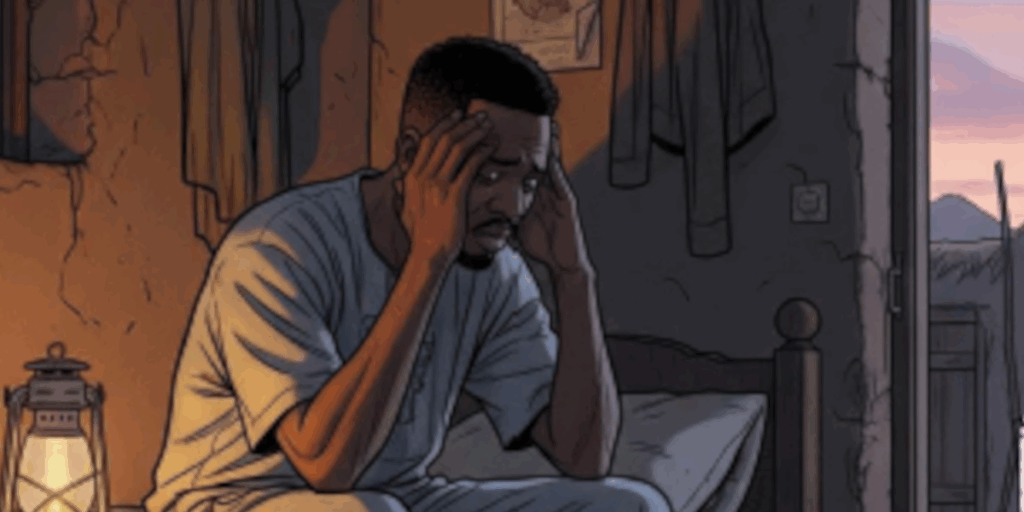
Human African trypanosomiasis, also known as sleeping sickness due to the uncontrollable drowsiness characteristic of its progression, is caused by the action of a parasite inoculated by the bite of hematophagous insects
It progresses in two stages: firstly infection of the blood, lymph and tissues, then impairment of the central nervous system that causes serious neurological and psychiatric disorders when the parasite crosses the blood-brain barrier. Without treatment, the infected person falls into a coma and eventually dies.
Two distinct forms of human African trypanosomiasis are widespread on the continent: one in West and Central Africa, caused by the Trypanosoma gambiense parasite. It progresses slowly, where infected people die after several years if they are not treated. It devastated these regions in the early 20th century, causing the death of millions of people before the discovery of treatments and implementation of large-scale health campaigns.
The other form, which is widespread in East Africa, is caused by Trypanosoma rhodesiense. Its progression is much faster: without appropriate treatment, patients die within only a few weeks, and even faster if they are not from a zone where the disease is endemic, such as tourists. Fortunately, this form is above all an animal disease, principally impacting wildlife and livestock, and affects few humans.
“Rhodesiense human African trypanosomiasis is a serious and fast progressing disease, that can impact all organs and requires urgent diagnosis and treatment. It is often incorrectly diagnosed, confused with malaria, to the detriment of patients”, states Lucille Blumberg, specialist in infectious diseases at the universities of Stellenbosch and Pretoria in South Africa.
There are no local cases of human trypanosomiasis in South Africa, but patients infected with Trypanosoma rhodesiense in Zimbabwe, Zambia and Malawi are treated there, mainly tourists or professionals such as hunters, wildlife administrators, ecologists, and scientists. Globally, the number of people infected every year is very low.
New treatment options
Until recently, available treatments were complex and onerous. For the first stage, when the parasite is still in the blood, lymph and tissues, molecules administered by intravenous or intramuscular injection had to be used. And as these molecules do not cross the blood-brain barrier, to combat the second stage of the disease, a lumbar puncture – a particularly unpleasant procedure – was required to determine whether the first- or second-line treatment should be used. This relied on melarsoprol, a molecule developed in the 1940s, also administered by intravenous injection, and which has the disadvantage of causing fatal encephalitis in nearly one in ten patients.
Recently, a new molecule has revolutionised the treatment of trypanosomiasis. Fexinidazole can in fact be administered orally, causes few adverse effects and, above all, is effective in treatment of both stages of the disease. This means there is no longer any need for lumbar punctures. It has already been evaluated, and adopted in WHO recommendations, for the treatment of trypanosomiasis caused by T. gambiense that is widespread in West and Central Africa.
Its effectiveness and good tolerance in treatment of T. rhodesiense still needed to be established. Now they have been. A clinical trial involving 46 patients in Malawi and Uganda – for which IRD trained healthcare personnel – confirmed this: the WHO now recommends its use instead of suramin and melarsoprol to treat both stages of this form of the disease.
“The introduction of oral fexinidazole represents significant progress in the treatment of rhodesiense human African trypanosomiasis, given the reactions that existed with melarsoprol,” concludes Veerle Lejon, who also contributed to drafting the WHO recommendations.
Olivier Blot